Antibiotic resistance is a huge challenge facing society globally, posing a threat not only to human health but in areas such as food security and the economy. The more we know about the mechanisms behind antibiotic resistance, the better we can respond to these threats.
New research, published in eLife, by scientists at the University of Oxford and Universidad Complutense de Madrid has confirmed that one of those mechanisms – driven by a sophisticated genetic system known as an integron – plays a key role in accelerating resistance and gives bacteria an ‘incredible opportunity’ to evolve in response to antibiotic treatment.
The new study highlights both the danger posed by integrons and the need to develop tools to counter their influence – for example, new drugs given alongside antibiotics that could limit an integron’s ability to accelerate bacterial evolution.
Lead author Dr Célia Souque, of Oxford’s Department of Zoology, said: ‘Antibiotic resistance is one of the biggest threats to modern medicine. As resistance grows, it will become harder to treat common infections such as food poisoning or pneumonia, or even to perform minor surgeries – and all parts of the world will be affected. We urgently need not only to develop new antibiotics, but to increase our understanding of how bacteria develop resistance to these treatments, with the aim of stifling the appearance of resistance in the first place.’
Integrons are genetic platforms found inside bacteria that allow bacteria to ‘shuffle’ antibiotic resistance genes carried within. This shuffling ability has been hypothesized to generate an important evolutionary advantage for bacteria, by allowing useful integron genes to be placed in more prominent positions, optimizing the levels of antibiotic resistance they provide.
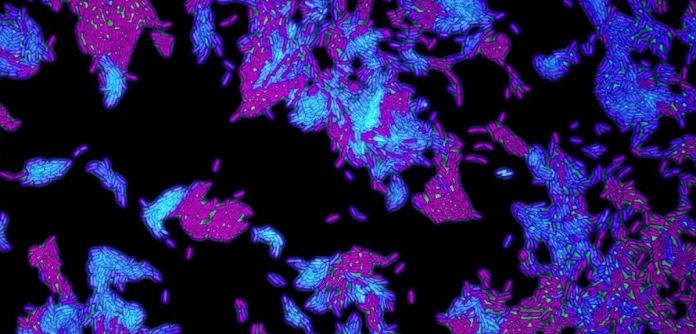
To probe experimentally for the first time the role played in resistance by integrons, the researchers inserted a customised integron carrying several resistance genes into a bacterium called Pseudomonas aeruginosa, which can cause pneumonia and blood infections in humans.
The scientists found that, when confronted with antibiotics, the P. aeruginosa bacteria with functioning integrons were able to survive longer than those without. Integron functionality was altered within the bacteria by retaining or removing integrase – the enzyme responsible for gene shuffling.
Dr Souque said: ‘Bacteria have multiple mechanisms to evolve resistance: they might mutate certain genes to dodge the effects of antibiotics, or acquire new genes that help produce antibiotic-destroying enzymes. But these mutations or novel genes often carry a cost, making the resistant bacteria less able to thrive than their non-resistant counterparts under normal conditions. Our results show that integrons give bacteria an incredible opportunity to evolve resistance “on demand”, while also using efficient gene shuffling to reduce the cost to the bacteria’s overall ability to thrive.’
Senior study author Professor Craig Maclean, also of Oxford’s Department of Zoology, added: ‘The integron is a remarkable genetic structure that is unique to bacteria – it provides them with a kind of Swiss army knife of antibiotic resistance genes that they can rapidly alter in response to our treatments.
‘Understanding the benefits that integrons provide to bacteria gives us insights into potential future treatment strategies to limit or counteract the evolution of antibiotic resistance. For example, antibiotics could be combined with molecules that inhibit integrase activity to reduce bacteria’s gene-shuffling ability and thus the evolution of higher levels of resistance.’