All cell membranes in the human body have embedded proteins that serve as sensors, messengers or as a means of transporting and regulating substances going in and out of the cell. Transport proteins in particular are poorly understood because of their structural complexity and their hydrophobic nature that makes them resistant to study. At the same time, these transport proteins, especially those that regulate glucose, play a vital role in the growth of cancerous tumors.
In a new study, scientists led by Dr. Shuguang Zhang, Ph.D. of the MIT Media Lab, demonstrate a method for quickly predicting the design of hydrophilic variant structures of the 14 glucose transport membrane proteins in cells. This will allow researchers to more easily study the proteins in water. The scientists confirm the accuracy of the predicted structures by comparing them to pre-existing crystallographic images of two of the proteins.
They hope that an enhanced understanding of these glucose transport proteins will hasten development of therapeutic monoclonal antibodies to treat cancer metastasis. This would essentially starve cancer cells by blocking glucose transporters.
“Most cancer cells significantly increase their expression and production of glucose transporters, called GLUTs, for their insatiable energy demand,” says Eva Smorodina, an undergraduate intern-student in structural biology at the Greiff Lab, University of Oslo, who is first author of a paper on the study published June 27 in QRB Discovery. “Currently there are almost no effective drugs to block GLUTs, since they have a challenging structure.”
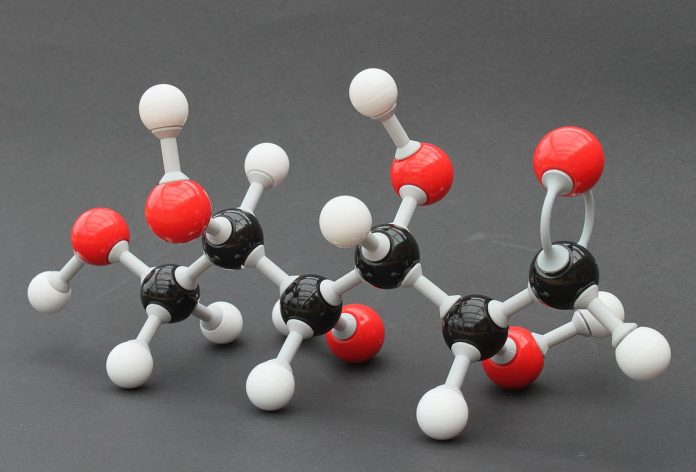
The GLUTs’ complex structures comprise 12 transmembrane hydrophobic helices embedded in the membrane. In their native or crystalline state, the hydrophobic structures must be placed in a special detergent or reagent for lab study, or they lose their structure. And with proteins, structure and function are indelibly related.
“Studying these proteins in detergent is like wearing heavy gloves to assemble an expensive watch or play a violin,” says Dr. Zhang, one of the few biomedical scientists for whom the study of membrane proteins is as compelling as it is vital to our understanding of cancer cells. He first began working on membrane proteins in the early 2000s. “Few people were studying these membrane proteins,” says Dr. Zhang. “They’re like a hot potato,” he says, because of their inherent resistance to study.
The new work is based on Dr. Zhang’s success four years ago, when he and a team accomplished what Dr. Zhang had been working on for nearly a decade: They designed a beautifully simple method called the QTY code for transforming a hydrophobic cell membrane protein into a hydrophilic protein by substituting many hydrophobic amino acids.
The QTY code is named for the symbols of the three amino acids — glutamine (Q), threonine (T) and tyrosine (Y) — that are substituted for four hydrophobic amino acids: leucine (L), isoleucine (I), valine (V) and phenylalanine (F). None of these amino acids carries a charge, which makes the substitution benign. Structure is essential to the functioning of the proteins, and the substitution doesn’t alter the structure.
In the latest study, Dr. Zhang and team apply the QTY code to the 14 glucose transport membrane proteins that transport sugar to cells. They used the new AlphaFold2 program, an artificial-intelligence based computational program developed by the company DeepMind, that can accurately and quickly predict how proteins fold. Dr. Zhang and team used the QTY code with the open-source AlphaFold2 to predict the alpha helical shapes of the 14 GLUT proteins in both their natural hydrophobic shapes and their QTY-code altered water-soluble shapes.
The crystalline or native state structures of two of the GLUTs — 1 and 3 — had been revealed previously by other researchers using X-ray crystallography. To substantiate their own methodology, Dr. Zhang’s team first predicted the hydrophilic structure of those two GLUTs by applying the QTY code’s amino acid replacements and letting AlphaFold2 predict the proteins’ shapes. It did so with great accuracy. The superposed hydrophobic and hydrophilic images are nearly identical.
The team followed up this confirmation by combining QTY code and AlphaFold2 to predict the hydrophilic structures of the 12 other GLUTs — in record time. “In 2018, it took four to five weeks using a high-speed computer cluster to simulate any protein structure,” says Dr. Zhang. “Now with AlphaFold2 we can use a Google computer for free, and it simulates the transmembrane proteins in hours. Some small proteins took less than an hour.”
“This study on human membrane glucose transporters and their water-soluble QTY variants from the Zhang laboratory at MIT is fascinating,” says Professor Joel Sussman of the Weizmann Institute of Science in Rehovot, Israel, who was not involved in the work. “It provides experimental visualization via X-ray crystallography and AI prediction using AlphaFold2 to see, for the first time, at atomic resolution, the differences between hydrophobic ‘water-hating’ helices and hydrophilic ‘water-loving’ helices. It is a critical step in using the QTY code method to study multispan transmembrane proteins and other aggregated proteins through their water-soluble variants, and is likely to have an enormous impact in the field of biotechnology.”
MIT Professor Robert Langer, whose work in biomedical engineering is highly celebrated, says, “The [QRB Discovery] paper is excellent, and I believe has the potential to help a lot of cancer patients.” Professor Langer was not involved in the research.
Authors of the QRB Discovery paper are Dr. Zhang and Smorodina; Fei Tao and Rui Qing of Shanghai Jiaotong University (Dr. Qing was previously a postdoctoral researcher in the MIT Media Lab and later a research scientist at the Koch Institute for Integrative Cancer Research at MIT); Dr. Steve Yang an MIT alumnus now at PT Metiska Farma in Indonesia; and Dr. David Jin, M.D., Ph.D. of Avalon GloboCare Corp., who stimulated Dr. Zhang to apply the QTY code to the study of cancer cells. Avalon GloboCare also funded the research.
Dr. Jin says he hopes — but this is not part of the current study — that future research will be able to genetically alter the glucose passage membranes to develop novel therapeutic targets.
“Now our only choices for cancer treatment are surgery, chemo or small-molecule therapy,” says Dr. Jin. “In future, it may be possible to take a patient’s T-cell, a component of the immune system, and genetically modify it in the lab so that it can work almost like a cancer-searching GPS system with a tumor-attacking capability.”