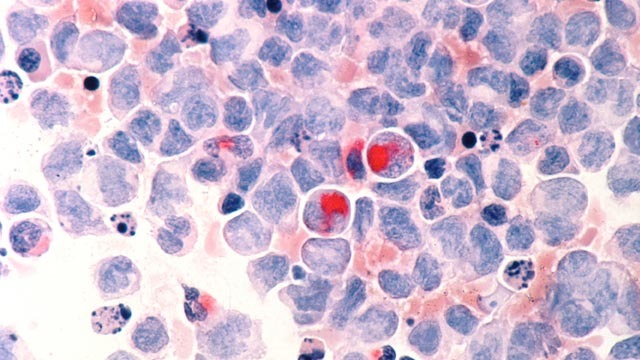
In myeloproliferative neoplasms, a form of chronic leukemia, the body constantly produces too many blood cells such as erythrocytes, platelets and granulocytes. This may lead to thrombosis, enlarged spleen and constitutional symptoms such as weight loss, bone pain and fatigue. The disease affects around one in a hundred thousand adults per year and, in the worst case, ends in acute leukemia with a short life expectancy.
The disease is triggered by mutations that cause the JAK2 tyrosine kinase to be permanently active, instead of only being activated when needed. This means that the bone marrow constantly receives signals to produce new blood cells. For about ten years now, inhibitors have been used that aim to limit the activity of JAK2.
The shortcomings of JAK2 inhibitor monotherapy
“The expectations we had for the treatment with JAK2 inhibitors have not been fully met,” says Professor Sara Christina Meyer, leader of the Myeloid Malignancies research team at the Department of Biomedicine at the University of Basel and Attending Physician in Hematology at the University Hospital of Basel (USB). While the symptoms improve, the proportion of leukemia cells in the blood remains high and after a few years the patients often no longer respond to the treatment. “We are addressing the question why this targeted therapy is not more effective.”
Her research team focuses on the MAPK signaling pathway, which is involved in the development of several cancers, and is controlled by JAK2 in myeloproliferative neoplasms. “We have found in previous studies that this signaling pathway remains active despite JAK2 inhibition, and continues to stimulate hematopoiesis,” said Professor Meyer.
To get to the root of the problem, the researchers therefore deactivated ERK1/2 – an important component of the MAPK signaling pathway – in addition to JAK2, and investigated whether such combined targeting works better in combating leukemia. They used three different test systems to do this: established leukemia cell cultures, mouse models for myeloid leukemia, and blood and bone marrow samples from patients. To deactivate ERK1/2, they used inhibitors that have recently become available and specifically block ERK1/2. One of the compounds, as well as an approved JAK2 inhibitor, were provided for the study by the company Novartis. In the mouse models, the researchers also deactivated the genes for ERK1/2 using molecular biology methods.
Combination works better to keep leukemia at bay
In all three test approaches, efficacy of JAK2 inhibitor treatment was enhanced when combined with the targeting of ERK1/2. This was seen by a reduction in blood cell production and (in the mouse model) reduction of spleen size. Meyer finds it particularly encouraging that combined treatment reduces the proportion of leukemia cells in blood and bone marrow, which is hardly ever the case with JAK2 inhibitors as single agents and could actually alter the disease course in the longer term.
Thanks to these promising results, the novel combination therapy approach has promptly been implemented into an international phase 1/2 clinical trial and is already being used in a small number of patients. Meyer expects first results in the next few months.
This important path from bench to bedside is very close to Meyer’s heart and, in her view, highlights the openness of the hematology field to innovation: “As a clinician and researcher, my focus is clearly on improving therapies. My main motivation is to find something that not only works in the dish, but can actually help people with leukemias such as myeloproliferative neoplasms.”