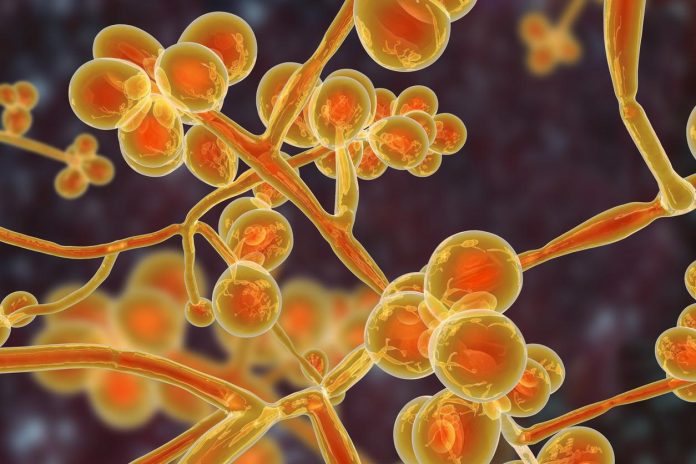
Candida auris is a fungus that has emerged as a major threat to public health in recent years. It is a type of yeast that can cause serious infections in humans, particularly those with weakened immune systems. The fungus is known for its ability to resist multiple antifungal drugs, making it difficult to treat. In this article, we will discuss how Candida auris is contracted and provide guidelines for its treatment.
Table of Contents
ToggleHow is Candida auris contracted?
Candida auris is primarily contracted in healthcare settings, such as hospitals and long-term care facilities. Patients who have a weakened immune system due to illness or medical treatment are at the highest risk of contracting the fungus. The fungus can spread through direct contact with contaminated surfaces or equipment, as well as from person to person.
The exact mechanisms of Candida auris transmission are not yet fully understood, but several factors may contribute to its spread. These include poor infection control practices, inadequate hand hygiene, and the overuse of antibiotics and antifungal drugs, which can promote the growth of drug-resistant organisms.
In addition to healthcare settings, Candida auris infections have also been reported in community settings, such as nursing homes and households. The fungus can survive on surfaces for weeks, making it easy to spread from one person to another.
Symptoms of Candida auris infection
The symptoms of Candida auris infection can vary depending on the site of infection. Common symptoms include fever, chills, and skin rash. In severe cases, the fungus can cause invasive infections, such as bloodstream infections, which can lead to sepsis and organ failure.
Diagnosis of Candida auris infection
Diagnosis of Candida auris infection can be challenging due to its similarity to other fungal infections. Laboratory testing is required to confirm the presence of the fungus. Healthcare providers should consider Candida auris as a possible cause of infection in patients with risk factors, such as recent hospitalization or exposure to healthcare settings.
Candida auris treatment guidelines
Previous studies report a prevalence of candidemia among colonized patients of around 17%, with an estimated cumulative incidence up to over 25% with increasing length of stay in critically ill subjects. Despite many reports of C. auris candidemia, coherent data on efficacy of active antifungal therapy are scanty, and hampered by small sample sizes, heterogeneity of treatment, and lack of adjustment for confounding factors. For example, many studies reported the use of antifungals with no in vitro activity. In two large Spanish studies, in which all strains were susceptible to echinocandins and echinocandins were included in the treatment regimen in all 41 and 47 patients, 30-day mortality was, respectively, 41% and 23%.
A necessary premise is that the prompt identification of C. auris colonization with the implementation of screening protocols in high-risk areas, and the subsequent put in place of adequate infection control measures to prevent cross-transmission of this pathogen among health-care facilities (such as contact precautions, cohorting or isolation of colonized patients) remain pivotal in the prevention of invasive C. auris infections, and thus of the consequent impact of C. auris on patients’ outcome. However, when C. auris candidemia develops, antifungal therapy should be promptly initiated. To date, echinocandins are the mainstay of C. auris candidemia treatment. Indeed, while resistance to fluconazole and polyenes may reach over 90% and 30%, respectively, resistance to echinocandins is around 5-7%, although important differences exist across studies (see Table 1) (Garcia-Bustos et al., 2021; Sanyaolu et al., 2022). High rates of MDR (intended as resistance to at least two classes of antifungals and reaching up to 25-50%) do jeopardize the possibility of second line treatments in patients who either fail or develop complications to first-line treatment with echinocandins (Garcia-Bustos et al., 2021; Sanyaolu et al., 2022; Vinayagamoorthy et al., 2022). In addition, biofilm production contributes significantly to hamper treatment of C. auris infections, through contributing to resistance to antifungals by efflux pumps or inhibition of drug diffusion, and by increasing the probability of persistent infection in case of inadequate source control (Sanyaolu et al., 2022).
There are worrisome reports of emerging resistance to echinocandins after a first treatment course with these antifungals, particularly in case of catheter-related infections (Biagi et al., 2019; Al-Obaid et al., 2022; Briano et al., 2022; Mulet-Bayona et al., 2022). These reports highlight how adequate source control is an essential intervention to improve treatment success and possibly prevent induction or selection of resistance (Biagi et al., 2019; Mulet-Bayona et al., 2022). Once again, however, a clear report of the number of patients who needed to switch to second line treatments is missing, although much needed to better understand the impact of antifungal resistance in clinical practice. For example, combinations of antifungals have been tested mostly in in vitro. Synergism was noted for echinocandins and azoles combinations, in particular for anidulafungin or micafungin and isavuconazole (Caballero et al., 2021), anidulafungin and isavuconazole (but not anidulafungin and voriconazole) (Caballero et al., 2021), and micafungin and voriconazole, while no synergy was observed for voriconazole and caspofungin (Fakhim et al., 2017). In vitro evidence of non-fungicidal activity of echinocandins monotherapy was also reported, supporting the interest in drug combinations (Caballero et al., 2021). No antagonism, but also no synergy (except for one strain), was reported for flucytosine-based combinations, including amphotericin B, micafungin and voriconazole (Bidaud et al., 2019; O’Brien et al., 2020). Synergy between amphotericin B and micafungin was demonstrated in 8 among 10 tested strains (Jaggavarapu et al., 2020). Of note, in addition to known limitations of in vitro synergy models, activity of drug combinations may be not only species-specific but also strain-specific (Caballero et al., 2021).
Novel drugs in clinical development
Some novel antifungal agents are in advanced phases of clinical development that, for the first time in years, could improve/expand spectrum of activity, route of administration, drug-drug interactions, tolerability of currently available antifungals (Rauseo et al., 2020; Hoenigl et al., 2021; Jacobs et al., 2021).
Rezafungin is a second generation echinocandin, administered intravenously once weekly thanks to its prolonged half-life (Sandison et al., 2017). Its activity against C. auris was investigated in two invasive candidiasis models of immunocompromised mice, in which rezafungin exhibited potent in vivo activity (Lepak et al., 2018) and performed better than amphotericin B or micafungin in terms of kidney tissue penetration (Hager et al., 2018b). A phase II randomized double-blind study (STRIVE), including 207 patients (none with C. auris infection), safety and efficacy of rezafungin was similar to caspofungin for treating candidemia and/or invasive candidiasis (Thompson et al., 2021). Very recently, the results of a noninferiority, double-blind study (RESTORE), comparing rezafungin vs. caspofungin for treating invasive candidiasis and/or candidemia have been released (Thompson et al., 2022). The 14-day overall cure (clinical cure, microbiological cure and radiological cure) in the modified ITT population was 60.6% (57/94) and 59.1% (55/93) in caspofungin-treated and rezafungin-treated patients, respectively (95% CI for difference -14.9 to 12.7).
Fosmanogepix (APX001), the prodrug of manogepix (APX001A, E1211), inhibits the inositol acyltransferase enzyme (Gtw1) involved in the trafficking and anchoring of mannoproteins on the fungal wall (Shaw and Ibrahim, 2020). It displays potent fungistatic activity against most pathogenic Candida spp., including C. auris (MIC90 ≤0.12 mg/ml), although not against C. krusei and C. kefyr (Miyazaki et al., 2011). The drug is available in both oral and intravenous formulations (Shaw and Ibrahim, 2020), distributes well to many difficult-to-treat body sites and shows a favorable drug-drug interaction profile. In a murine model of disseminated C. auris infection, survival was 80-100% and 50% in fosmanogepix-treated and anidulafungin-treated animals, respectively (Hager et al., 2018a). In a phase II, single arm study, including 21 non-neutropenic patients with candidemia treated with fosmanogepix, success rate was 80% (16/20) (Pappas et al., 2020). Among nine critically ill subjects with C. auris candidemia, treatment success at end of fosmanogepix treatment and 30-day survival were both 89% (Kullberg et al., 2021).
Ibrexafungerp (SCY-078 or MK-3118) is a 1,3-beta-D-glucan synthase inhibitor with fungicidal activity against Candida spp., including C. auris (Ghannoum et al., 2018). Compared to echinocandins, ibrexafungerp binds a different site of the same target, so cross-resistance is limited (Jimenez-Ortigosa et al., 2017). Differently from echinocandins, ibrexafungerp is administered orally. An intravenous formulation has also completed phase 1 of clinical development (SCYNEXIS, 2021). In preclinical models, ibrexafungerp was shown to improve survival of neutropenic mice with C. auris invasive candidiasis (Wiederhold et al., 2021). In recently published phase II study, oral ibrexafungerp following initial echinocandin therapy was compared to standard of care (step-down to fluconazole) in non-neutropenic patients with invasive candidiasis. Favorable clinical response was 71%, 86%, and 71% in patients receiving ibrexafungerp 500 mg, ibrexafungerp 750 mg, and fluconazole (Spec et al., 2019). One phase III open-label study (CARES, NCT03363841) specifically evaluating the safety and efficacy of ibrexafungerp for C. auris infection is currently ongoing. In the first ten patients enrolled, complete response was 80% (Juneja et al., 2021). Other studies assessing the safety and efficacy of oral ibrexafungerp for invasive candidiasis are currently ongoing (FURI, NCT03059992 and MARIO, NCT 05178862).