Biomedical scientists at the University of California, Riverside, propose a way for drugs to be more effective against inflammatory bowel disease, or IBD, in which the intestine undergoes inflammation.
IBD, a chronic inflammatory disease of the intestine, includes Crohn’s disease and ulcerative colitis. It is commonly treated with one of several available biological drugs that block an inflammatory molecule called Tumor Necrosis Factor Alpha, or TNF-alpha, from binding to two receptors, TNFR1 and TNFR2. Only about 50% of patients are helped long term by this treatment.
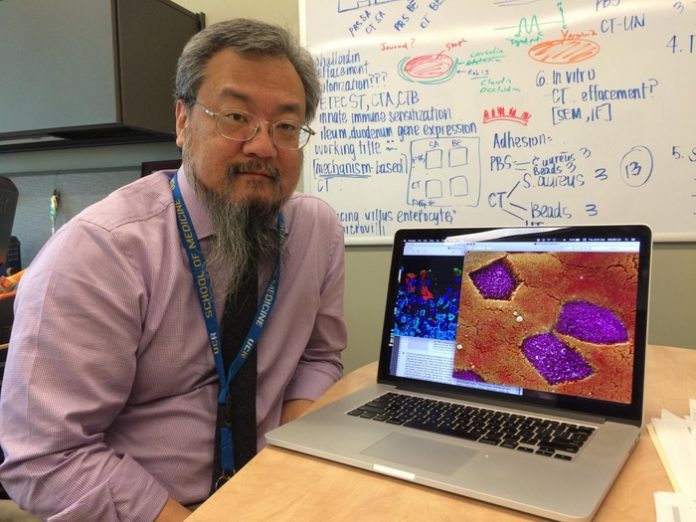
“TNF-alpha does drive much of the inflammation and tissue destruction in IBD,” said Dr. David D. Lo, a distinguished professor of biomedical sciences in the School of Medicine, who led the study appearing in the Journal of Crohn’s and Colitis. “It’s why it is targeted by drugs. Our interest in this study was to look for a more targeted therapy that might have better impact than the existing approach, which is to block all TNF-alpha.”
Lo explained that people have two different receptors, TNFR1 and TNFR2, in each of their cells that bind TNF-alpha. Currently, TNF-alpha-targeted drugs block both TNFR1 and TNFR2. Lo’s experiments were done in mice, which have the same two receptors. The pattern of inflammation in mice is similar to that seen in humans.
TNF-alpha, produced by the body’s cells, also induces specialized immune and other cells, which both promote inflammation and suppress it. Thus, TNF-alpha plays a role in the destruction and the healing of tissues — a double-edged sword. Lo said evidence exists that TNFR1 may be driving most of the destructive effects of IBD, whereas TNFR2 may drive the healing and restorative effects.
“If you block both the receptors, you block the destructive effects and the recovery,” he said. “To circumvent this, in our work we opted to do selective targeting of TNFR1.”
Lo’s group was encouraged by two pieces of evidence suggesting that targeting TNFR1 may be a more beneficial strategy. The researchers used a reagent from INmune Bio, a biotechnology company, that was selective for blocking TNFR1. Mice treated with this reagent were found to benefit from it. The researchers also did genetic targeting of TNFR1 to reduce its signaling. The impact, they found, was dramatic.
“When we reduced TNFR1 signaling, the mice showed a significant benefit relative to mice who had the full level of TNFR1 signaling,” Lo said. “This approach may offer more opportunity to TNFR2 to contribute to the healing.”
According to Lo, mice that have a genetic deficiency in TNFR2 get much more severe disease, suggesting that TNFR2 does indeed have beneficial effects.
“Without TNFR2, IBD is a lot worse,” he said.
Several diseases, such as rheumatoid arthritis, multiple sclerosis, and psoriasis, are related to the action of TNF-alpha. Indeed, different tissues in the body are differently sensitive to the effects of TNF-alpha. The role of the receptors TNFR1 and TNFR2 varies in the different tissues.
“TNF-alpha is a very common way in which your body reacts to inflammatory triggers, such as infection,” Lo said. “This protein can mediate several processes in the body to promote inflammation. The inflammation arises to clear an infection or kill a tumor. But in autoimmune diseases, the same inflammation and tissue damage that TNF-alpha provokes are what drive the disease. In other words, you want TNF-alpha at the right time to knock off a certain infection but once that is accomplished, you don’t want this protein to be around any longer. Many diseases are linked to TNF-alpha lingering in tissues.”
Lo said the current research was a combination of testing approved drugs that are used in the clinic as well as examining more detailed questions related to the mechanisms of disease and protection.
“It’s about continuously finding better cutting-edge drugs and better targets to treat diseases,” he said.
Lo was joined in the study by Rajrupa Chakraborty, Mia R. Maltz, Diana Del Castillo, Purvi N. Tandel, Nathalie Messih, and Martha Anguiano.